About Interstitial lung diseases (ILD)
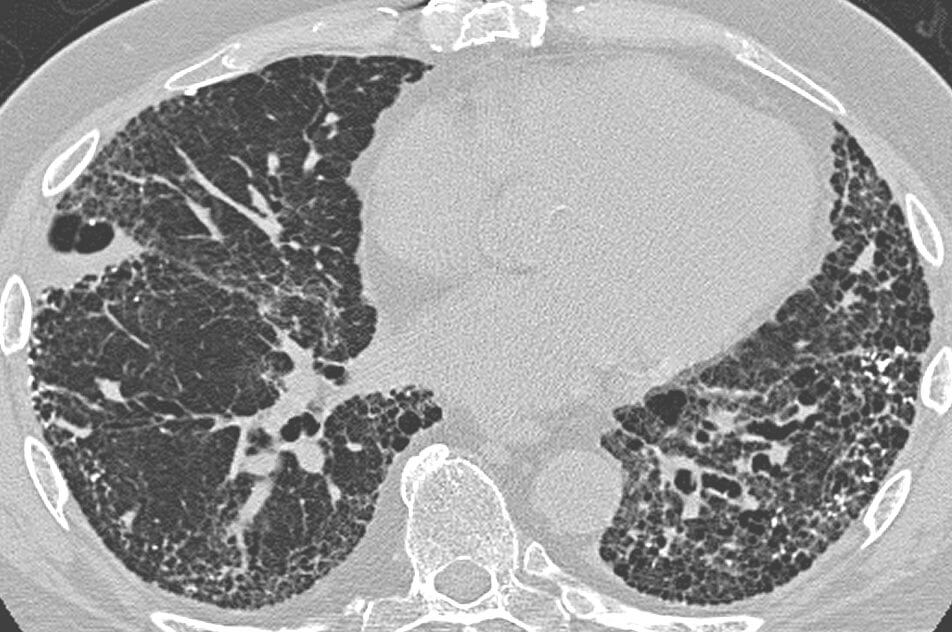
Interstitial lung diseases (ILD) also called Diffused parenchymal lung diseases (DPLD) are a group of diseases which are characterized by bilateral, patchy pulmonary fibrosis. In these diseases mainly the alveoli, interstitial spaces, basement membrane, alveolar epithelium, interstitial vasculature, perivascular and perilymphatic tissues are affected. Damage to concerned sites lead to abnormal ventilation-perfusion ratio which further leads to hypoxia. In such conditions, the physicians conduct a chest radiograph to observe typical ground-glass shadows. The characteristic pathologic and histologic features categorize the diseases falling under ILD. If prompt measures are not taken the condition of patient can worsen causing scarring and gross destruction of lung. Respiratory failure, pulmonary hypertension and cor pulmonale are common complications. In end stage, the lung is called honey-comb due to its gross appearance.

Figure 1: Honeycomb Lungs
Interstitial Lung Disease Causes
Interstitial Lung Diseases are caused by wide range inhalants, medical conditions as well as idiopathic backgrounds can trigger a series of abnormal events for the healing process. These inhalants include silica dust, asbestos fibers, grain dust, animal droppings, coal dust, metal dust, talc and radiation treatments. Other than inhalants medical conditions like rheumatoid arthritis, scleroderma, sarcoidosis, Sjogren’s syndrome and mixed connective tissue disease can damage lungs. In order to recover, body produces tissue to repair the damage. Repeated healing mechanisms lead to accumulation of tissue around alveoli making them thick and scarred. This ultimately leads to difficulty in gaseous exchange at the site of alveoli due to which tissues receive insufficient supply of oxygen.
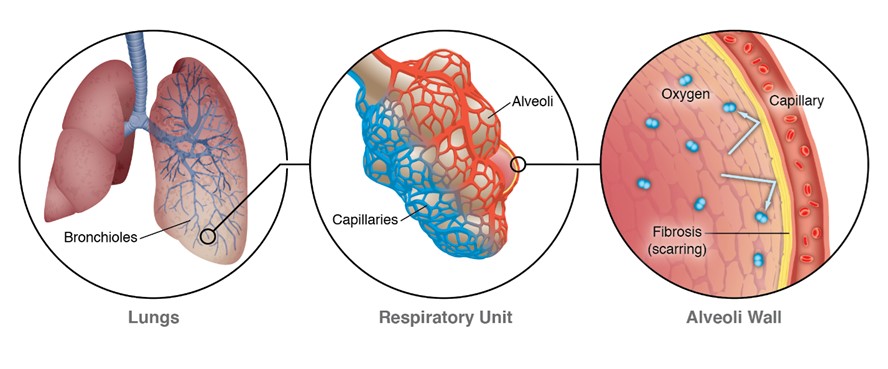
Figure 2: https://www.nationaljewish.org/conditions/interstitial-lung-disease-ild/ild
Interstitial Lung Disease Symptoms
As soon as ILD happens to an individual the symptoms take some time to appear unless it is acute interstitial pneumonitis. As compared to other ILD in this disease shortness of breath occurs within few hours or days. Shortness of breath is accompanied with worsening cough and weight loss. As the time progresses, the symptoms worsen. Unfortunately, when the symptoms first appear enough irreversible lung damage is already done. Even then it is necessary to consult a doctor.
The pathologic and histological findings classify them into following diseases;
- Interstitial pneumonia; most commonly caused by bacteria called Mycoplasma pneumonia.
- Idiopathic pulmonary fibrosis; thick scar tissue grows in the interstitium.
- Non-specific interstitial pneumonitis; often affects the individuals fighting with autoimmune disorders such as rheumatoid arthritis.
- Hypersensitivity pneumonitis; usually occurs in individuals who inhale mold, dust, silica, coal dust for a long period of time.
- Cryptogenic organizing pneumonia; a specific kind of pneumonia in which no infection takes place.
- Acute interstitial pneumonitis; severe and fatal lung disease in which the patient is often kept alive with the help of a ventilator.
- Desquamative interstitial pneumonitis; typically results from smoking.
Interstitial Lung Disease Complications
Severe and untreated ILD can lead to quite harsh complications. Most commonly observed complications include;
- Pulmonary hypertension
The scarring severely affects the arteries in lungs due to which blood flow is restricted.
- Cor pulmonale
The right ventricle experiences increased strain to pump blood due to pulmonary hypertension. This is often called “Right heart failure”.
- Respiratory failure
The blood oxygen level is too low which causes increased pressure in pulmonary arteries. Force exerted by right ventricle multiplies leading to heart failure.
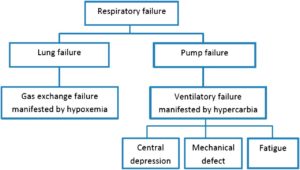
Figure 3: https://pedsinreview.aappublications.org/content/35/11/476
Interstitial Lung Diseases (ILD) can be treated with adequate attention. Medicines, pulmonary rehabilitation, oxygen therapy and lung transplant are active treatment options depending upon the severity of condition.
FAQS About Interstitial Lung Disease (ILD)
Here are some frequently asked questions (FAQs) about Interstitial Lung Disease (ILD):
What is Interstitial Lung Disease (ILD)? Interstitial Lung Disease (ILD) is a group of disorders that cause inflammation and scarring of the lung tissue, specifically the interstitium, which is the space between the air sacs in the lungs. This can lead to difficulty in breathing and reduced lung function.
What causes ILD? ILD can have various causes, including autoimmune disorders, environmental exposures (such as asbestos or certain chemicals), medications, infections, and idiopathic (unknown) causes. Some common types of ILD include idiopathic pulmonary fibrosis (IPF), sarcoidosis, and connective tissue disease-associated ILD.
What are the symptoms of ILD? Symptoms of ILD can include shortness of breath, persistent dry cough, fatigue, chest discomfort or pain, weight loss, and in later stages, clubbing of the fingers and toes.
How is ILD diagnosed? Diagnosis often involves a combination of medical history review, physical examination, pulmonary function tests, chest X-rays, CT scans, and sometimes lung biopsies. These tests help doctors determine the type and severity of ILD.
Is ILD treatable? Treatment options depend on the underlying cause and type of ILD. In some cases, addressing the underlying cause (such as stopping exposure to harmful substances) can slow down the progression. Medications, oxygen therapy, pulmonary rehabilitation, and lung transplantation are also potential treatment approaches.
Can ILD be cured? While there is no cure for most types of ILD, early diagnosis and appropriate management can help slow the progression of the disease, improve quality of life, and manage symptoms.
How does ILD affect lung function? ILD causes inflammation and scarring of the lung tissue, which leads to reduced lung elasticity and capacity. This makes it harder for the lungs to expand and contract, resulting in reduced lung function and difficulty in getting enough oxygen into the bloodstream.
Is ILD the same as pulmonary fibrosis? Pulmonary fibrosis is a type of ILD. It specifically refers to the scarring (fibrosis) of the lung tissue. There are various causes of pulmonary fibrosis, and it can be a result of different types of ILD.
Who is at risk for developing ILD? People who are exposed to certain environmental factors (like occupational dust or chemicals), have a history of autoimmune diseases, smoke, or have a family history of ILD are at a higher risk of developing the condition.
Is ILD contagious? No, ILD is not contagious. It is a result of internal factors such as autoimmune reactions, genetics, or environmental exposures rather than being caused by a contagious agent.
Can lifestyle changes help manage ILD? Lifestyle changes such as quitting smoking, maintaining a healthy weight, staying physically active within your limitations, and avoiding exposure to pollutants can positively impact the management of ILD.
Remember, if you suspect you or someone you know might have ILD, it’s important to consult a medical professional for proper diagnosis and treatment recommendations
CT scan in a patient with usual interstitial pneumonia, showing interstitial thickening, architectural distortion, honeycombing and bronchiectasis.
https://en.wikipedia.org/wiki/Honeycombing
NOVA Pulmonary Critical Care and Sleep Associates is committed to providing excellent care in all aspects of Pulmonary Medicine and Sleep Disorders. With offices located in Lansdowne and Dulles/South Riding, we offer care for the entire Northern Virginia region, serving locations from Chantilly, Fairfax, Centreville, Manassas, Gainesville to Reston, Sterling, Leesburg, Ashburn, Arlington, Alexandria Brambleton, Purcellville and more.



Office Locations
Conveniently located near you in Loudoun and Fairfax VA
NOVA Pulmonary – Dulles
24430 Stone Springs Boulevard
Suite 200
Dulles, VA 20166
NOVA Pulmonary – Lansdowne
19415 Deerfield Avenue
Suite 301
Landsdowne, VA 20176